ADHD vs BPD
ADHD vs. BPD
Since week one of my ADHD #misdiagnosismonday series, I’ve consistently received requests to cover ADHD vs. Borderline Personality Disorder (BPD). I must admit I have been procrastinating. After doing Autism and BPD, I appreciated the complexity I’d be diving into, so I wanted to wait until I had some bandwidth to dive in and give it the proper attention it deserved.
The Complex Connection Between ADHD and BPD
It turns out I wasn’t wrong. It is complex. It is complex for many reasons; the primary reasons for the complexity include:
1) ADHD and BPD co-occur at high rates (higher than the general population)
2) They share key clinical and temperamental similarities
3) They share similar genetic and developmental pathways (Weiner et al., 2019).
Overview of BPD and ADHD
BPD is classified as a personality disorder and traditionally was not diagnosed until adulthood (it was recently updated and can now be diagnosed in adolescence). It is diagnosed in females more often and is characterized by “impairment in interpersonal functioning (including poor empathy, problems with trust and intimacy), and difficult personality traits, such as disinhibition and antagonism, and impulsivity” (Botbol, 2017).
ADHD, on the other hand, is categorized as a neurodevelopment disorder, and traits must be present before age 12. ADHD is characterized by “a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development” (APA, 2013).
Overview of Borderline Personality Disorder
Borderline Personality Disorder (BPD) results from the interaction between biological and psychosocial factors. It is thought to occur as a result of a sensitive genotype + invalidating childhood environment (Weiner et al., 2019). When temperamental traits, such as impulsivity and emotional dysregulation, merge with an invalidating environment, children struggle to regulate their emotions, which can result in extreme emotional vacillations and the development of BPD (Weiner et al., 2019).
BPD is defined as a “pervasive pattern of instability of interpersonal relationships, self-image and affects, and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by 5 (or more) of the following”:
1. Frantic efforts to avoid real or imagined abandonment.
2. A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
3. Identity disturbance: markedly and persistently unstable self-image or sense of self.
4. Impulsivity in at least 2 areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating).
5. Recurrent suicidal behavior, gestures or threats, or self-mutilating behavior.
6. Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days).
7. Chronic feelings of emptiness.
8. Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
9. Transient, stress-related paranoid ideation or severe dissociative symptoms.
Source: DSM-5 Criteria, can be accessed in Biskin and Paris article
Overview of ADHD
ADHD is classified as a neurodevelopment condition, meaning the onset occurs during the developmental period (typically early childhood) and has a strong genetic component. The parts of the brain that regulate emotions, attention, and focus are impacted in the context of ADHD.
ADHD is characterized by difficulty regulating inattention, hyperactivity, and impulsivity (American Psychiatric Association 2013). The criteria for diagnosing ADHD include the presence of inattention, impulsivity, and hyperactivity (or just inattention in the case of ADHD-inattentive type). These characteristics must interfere with daily functioning in at least two contexts (for example, home and school or work and home) (American Psychiatric Association, 2000).
Some common traits of ADHD include:
difficulty focusing or staying on task
problems keeping track of materials
trouble following through on complex projects
distractibility and forgetfulness
appearing not to listen when spoken to
increased need to be up and moving
fidgetiness
impulsivity
tendency to interrupt other people
excessive talking
While present from birth, ADHD may not become apparent until demands exceed capacity. And many children develop sophisticated compensatory strategies to offset areas of struggle. In these cases, ADHD may not be recognized until late in life.
ADHD is the most common childhood psychiatric condition, with an estimated prevalence of 2% to 15% (Robertson, 2008). ADHD has a worldwide prevalence of 5.2 % among children and adolescents (Polanczyk et al. 2007). Based on the (CDC), current estimates estimate that 6.1 million children in the U.S. are diagnosed with ADHD, approximately 9.4% of children, making ADHD one of the most commonly diagnosed developmental conditions in the U.S.
Prevalence of Co-Occurrence
BPD occurs more frequently within the ADHD population than would happen by chance and vice versa (ADHD in BPD population). (Weiner et al., 2019). When they occur together, it is possible for one diagnosis to be missed. More often, the “louder” symptoms of BPD may mask the “quieter” traits of ADHD.
Women whose ADHD is missed at higher rates (than men) are particularly vulnerable to having their ADHD missed when they are experiencing both conditions. Due to variance across studies, it can be difficult to get an accurate sense of co-occurrence. Here is a summary of some of the current findings (you will notice a lot of variances):
Prevalence of BPD among ADHDers
In a population sample, 33.7% of ADHDers were found to have a lifetime prevalence of BPD (compared to a 5.2 prevalence rate in the general population) (Bernardi et al., 2012)
In a large-scale population study done in Sweden, ADHDers had 19.4 times higher odds of BPD diagnosis than individuals not diagnosed with ADHD (Kuja-Halkola et al., 2018).
Jacob et al., 2007 found at least 14% of individuals diagnosed with ADHD in childhood later receive a diagnosis of BPD.
Between 18%-34% of adult, ADHDers are estimated to have co-occurring BPD (Matthies et al., 2011; Rasmussen and Gillberg, 2000).
In a longitudinal study, Miller et al., 2008 found that children diagnosed with ADHD between 7-11 were significantly more likely to be diagnosed with BPD at the 16-26 year follow-up than non-ADHDers (13.5% likelihood vs. 1.2%).
In another longitudinal study involving two cohorts of girls Stepp et al, 2012 found higher levels of ADHD and Oppositional Defiant Disorder (ODD) scores at age 8 predicted BPD symptoms at age 14.
ADHD women, especially those with combined type, are more likely to have BPD than ADHD men, who are more likely to be diagnosed with antisocial personality disorder (Cumyn et al., 2009).
Prevalence of ADHD among individuals with BPD
In a meta-analysis Ditrich et al., 2021 found the prevalence of ADHD in BPD individuals to be 30%-60% (However, it should be noted many studies found smaller percentages.
Fossati et al., 2002 found that 60% of patients with BPD had WURS-25 scores suggestive of childhood ADHD
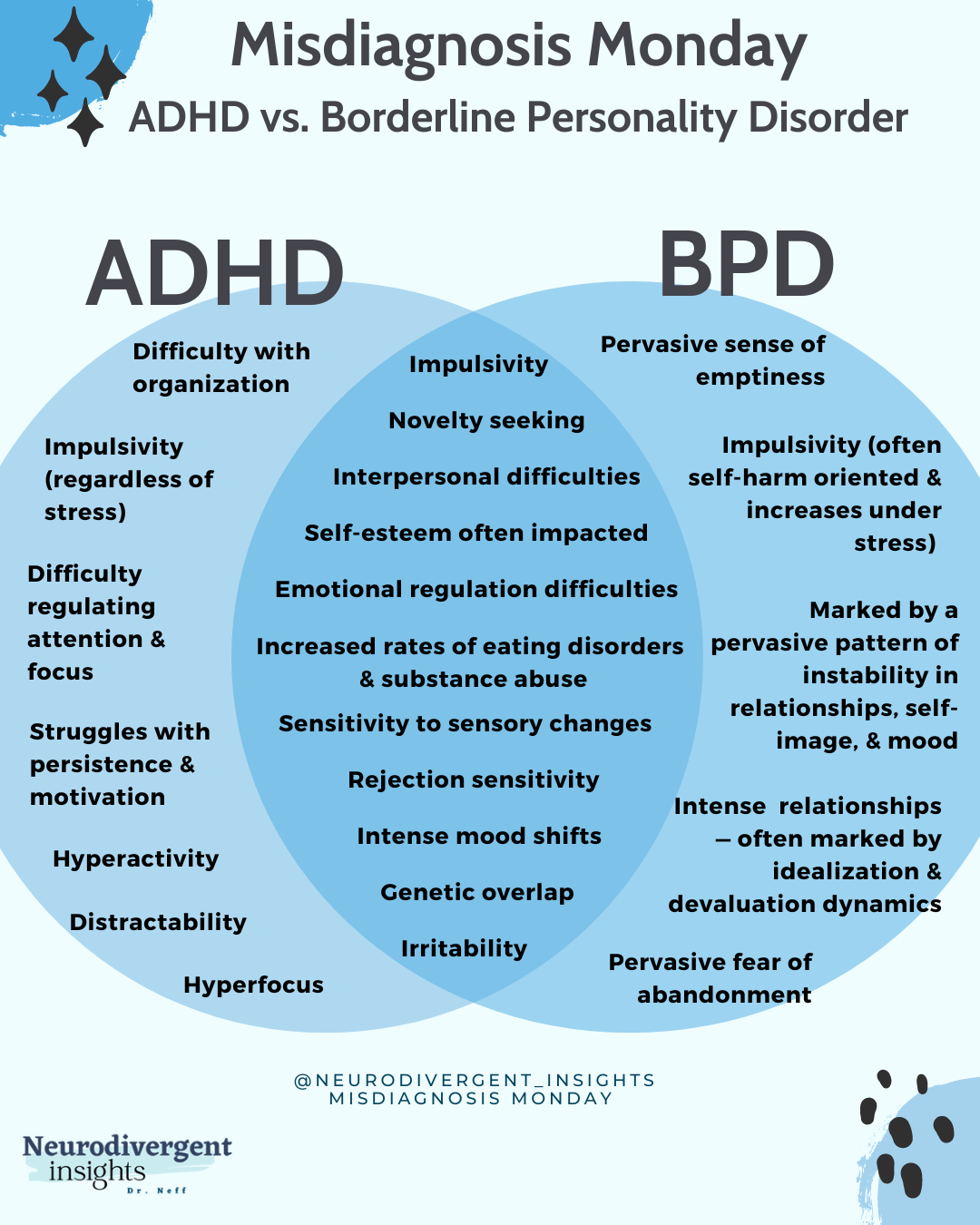
Overlapping Traits and How to Spot the Difference
ADHD and BPD share many temperamental similarities, symptoms, and traits, making it challenging for clinicians to distinguish the difference. When both conditions are present, it is possible that the "more dramatic BPD symptoms can camouflage the more classic ADHD symptoms" (Littman, 2021).
If an adult has evaded ADHD diagnosis in childhood problematically, the possibility of ADHD may not be on a clinician's radar. Littman, 2021 hypothesizes that because ADHD was rarely diagnosed in inattentive women until relatively recently, many lived with a misdiagnosis of BPD.
Clinically, both groups may present similarly in adolescence and adulthood as both are characterized by difficulties in self-regulation, feelings, behavior, relationships, and sense of self (Littman, 2021). Both groups are hypersensitive to sensory changes and experience key challenges with impulsivity and emotional regulation.
For both groups, impulsivity can result in financial strain, addiction, gambling, unsafe sex practices, eating disorders, and risky behavior (Littman, 2021). And in both conditions, struggles with regulating emotions can lead individuals "to feel ashamed, unsupported, and alone, struggling with anxiety, depression, rage, panic, and despair" (Littman, 2021). The key clinical symptom overlap includes impulsivity and emotional dysregulation. Beyond that, both conditions are also associated with interpersonal struggles and temperamental similarities (Weiner et al., 2019).
Temperamental Overlap
ADHD and BPD share several traits, particularly novelty seeking and harm avoidance (Weiner et al., 2019).
Novelty Seeking
Novelty seeking (a strong interest in having new experiences) is high among both groups. van Dijk et al., 2012. The highest novelty-seeking scores were found among the ADHD+BPD group.
Harm Avoidance
Both groups also have a large level of harm avoidance (Weiner et al., 2019). Harm avoidance is characterized by excessive worrying, pessimism, shyness, fearfulness, doubt, and being easily fatigued. It is also associated with reduced serotonin (Chen et al., 2015).
Clinical Symptom Overlap
The two core features that ADHD and BPD share include impulsivity and emotional regulation difficulties (Ditrich et al., 2021; Weiner et al., 2019).
Impulsivity (Similarities and Differences)
Impulsivity is a core feature of both conditions. Impulsivity has been identified as one of the dimensions having the greatest overlap between ADHD and BPD in adults. Both ADHD and BPD individuals report higher levels of trait-impulsivity compared to controls when using self-report measures such as the Barratt Impulsiveness Scale (BIS) (Weiner et al., 2019).
Impulsivity is defined as action taken without reflecting on the consequences or acting out of spontaneous impulses without thinking about consequences (Ditrich et al., 2021). While impulsivity is a key feature of both ADHD and BPD, they also have some subtle differences which can help to distinguish the conditions from one another.
Diagnostic criteria for these two conditions define and look at impulsivity differently. Impulsivity, in BPD, typically refers to impulsive self-harm. Whereas impulsivity in ADHD is typically in reference to interrupting others, having difficulty waiting for one's turn, talking over people, and interrupting what other people are doing. (Ditrich et al., 2021). Note impulsive self-harm can occur in the context of ADHD as well; however, it is not included as part of the diagnostic criteria and is not always present.
Studies looking at impulsivity using neuropsychological assessments found some interesting differences (research findings summarized in Ditrich et al., 2021):
Individuals with BPD had more difficulty using context cues for inhibiting responses, and their impulsivity was stress-dependent (which became worse when under stress). Alternatively, ADHDers had more motor impulsivity (difficulty stopping an action that was already in motion).
Individuals with both ADHD + BPD had the highest rates of impulsivity.
Two studies found impaired inhibition to be a core feature of adult ADHD but not in adults with BPD. In the context of BPD, inhibition impairment has mainly been observed in the context of "emotionally-conditioned tasks" (i.e., stress). This suggests different pathways to inhibition. While ADHD is associated with difficulties with top-down executive functioning processes, BPD has more to do with emotional dysregulation (Weiner et al., 2019).
While the comparative data on impulsivity in ADHD and BPD is still relatively scarce. Based on current results, impulsivity in BPD is intrinsically related to emotional dysregulation (meaning in high-stress situations, individuals with BPD have more pronounced impulsive behaviors), while ADHD impulsive behaviors are less stress-dependent (Weiner et al., 2019). Overall, trait impulsivity is higher among ADHD and ADHD+BPD groups than the BPD group only group. (Weiner et al., 2019). A clinician should observe if impulsivity occurs only in the context of stress (particularly relational stress) or is more global in nature.
Emotional Regulation (Similarities and Differences)
Difficulty regulating emotions is a key component of BPD and is addressed in at least two of the DSM-5 criteria. Although it is not officially included in the core diagnostic criteria for ADHD, emotion dysregulation is consistently seen among ADHDers, and it has been argued that it should be added as a key component of ADHD. Up to 70% of adult ADHDers experience difficulties with emotional regulation (Weiner et al., 2019). Many consider this to be a primary feature of ADHD (Ditrich et al., 2021; Hirsch et al., 2018 ).
In a study involving 279 ADHDers, 70 individuals with BPD and 60 individuals with ADHD+BPD, and a group of controls. The following finders emerged Rüfenacht et al., 2019:
All clinical groups (ADHDers and BPD) had high emotional reactivity, including emotional sensitivity, intensity, and persistence of emotions.
The highest rates were found among those with both ADHD and BPD. Followed by BPD only, followed by ADHDers only.
Overall trait emotional dysregulation is highest in BPD and BPD +ADHD groups. ADHDers had better control over their emotions, less emotional reactivity, and used more adaptive cognitive strategies than BPD individuals (however still had more emotional regulation difficulties than the control group).
Physiological Similarities: Similar physiological responses to emotions have been observed among both groups. In both groups, individuals experience negative emotion/stress/tension for a longer duration of time and are slower to respond to their baseline following an emotionally arousing experience (Weiner et al., 2019.) This is what I, at times, refer to as the "rigid neurodivergent nervous system." Our nervous systems tend to be less flexible and adaptable. The research findings suggest folks with ADHD and BPD experience more emotional stress and have more difficulty returning to their baseline.
Causes of Stress: While the bodily stress response may be similar, one way to tease out the difference is to look at the cause of stress. While ADHDers are more likely to experience emotional stress, shame, and despair associated with choices or perceived failures (related to executive functioning challenges), individuals with BPD are more likely to experience emotional stress related to perceived abandonment or stressors in relationships, which can lead to a sense of hopeless and frantic panic (Littman, E., 2021).
Inattention
Inattention can also be experienced in the context of BPD. However, it often occurs in the context of dissociative experiences (Asherson et al., 2014). This can make it difficult to tease out ADHD inattentive/daydreaming from dissociative symptoms (particularly if relying on screeners) (Littman, E., 2021). Given that most women diagnosed with ADHD have ADHD-inattentive type, this may mean ADHD-inattentive women are more likely to be misdiagnosed with BPD. To tease out the difference, a clinician would want to discern if inattention was occurring secondary to dissociative or was more globally present.
Interpersonal Problems
Both conditions are associated with interpersonal problems. However, they appear to have different underlying mechanisms contributing to interpersonal difficulties (Weiner et al. 2019). In the context of BPD, interpersonal challenges are often characterized by unstable and intense relationships that shift between idealization and devaluation. There is also marked interpersonal sensitivity with extreme efforts (often interpreted as manipulation) to avoid abandonment (Weiner et al. 2019).
The underlying causes of interpersonal challenges within ADHD have been less studied. However, it has been conceptualized that relationship challenges are related to the core triad of symptoms (inattention, impulsivity, and hyperactivity). Additionally, inattention may contribute to social-communication difficulties. Such relationship difficulties can thus be seen in the context of executive functioning difficulties, while BPD relationship difficulties are better understood in the context of emotional regulation difficulties (Weiner et al. 2019).
Distinguishing Clinical Markers
Experiences that would be consistent with BPD but not ADHD include: frantic efforts to avoid real or imagined abandonment, suicidal behavior, self-harm, chronic feelings of emptiness, and stress-related paranoia/severe dissociation (Asherson et al., 2014)
Dowson et al., 2004 found inattention, lack of organization, and persistence distinguished ADHD from BPD, whereas interpersonal impairment did not.
Implications for Treatment and Future Research
Screening tools lack discriminative power in clinical settings, probably due to shared symptomatic expressions (e.g., emotion dysregulation and impulsiveness). Given high symptom and trait overlap and high rates of co-occurrence, a clinician should be well-versed in both conditions when assessing ADHD or BPD. As Weiner et al., 2019 observes:
“despite the importance of screening for ADHD in the context of BPD (and vice-versa), screening tools lack the ability to discriminate ADHD in BPD patients and to our knowledge, the psychometric properties of BPD screening measures in adult ADHD have yet to be investigated. Therefore, clinicians should not rely on screening measures alone to make a diagnosis; instead, clinicians working in each field (BPD and ADHD) should be knowledgeable of the other field in order to effectively detect comorbid cases in clinical practice, based on the careful intake of the patient’s psychiatric and developmental history.
2. Clinicians should be cautious of over-relying on “age of onset.” While this used to be a factor that distinguished ADHD from BPD, emerging research places this form of distinction under question. Weiner et al., 2019 suggest that Adult ADHD and BPD can no longer be viewed as purely early-onset neurodevelopment and late-onset psychological disorders (BPD). There is a need for further understanding of sensitive genotypes, environment, and adverse childhood experiences to distinguish the disorders from a developmental vs. clinical framework. As Weiner et al., 2019 notes:
Of major importance, age of onset used to be a discriminative diagnostic criterion between ADHD, typically viewed as an early-onset neurodevelopmental disorder, and BPD, a late-onset psychological disorder. However, this distinction has been recently called into question, increasing the need for more research aiming at delineating the disorders from a developmental and clinical standpoint.
3. More research is needed to help identify children at risk for both ADHD and BPD to create more effective interventions and support (Weiner et al., 2019).
4. More research is needed to determine the effectiveness of treatment for BPD+ADHD (both psychological and pharmacological interventions) (Weiner et al., 2019).
Citations
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington: American Psychiatric Publishing; 2013. https://doi.org/10.1176/appi.books.9780890425596.
Anckarsäter, H., Stahlberg, O., Larson, T., Hakansson, C., Jutblad, S. B., Niklasson, L., Nydén, A., Wentz, E., Westergren, S., Cloninger, C. R., Gillberg, C., & Rastam, M. (2006). The impact of ADHD and autism spectrum disorders on temperament, character, and personality development. The American journal of psychiatry, 163(7), 1239–1244. https://doi.org/10.1176/appi.ajp.163.7.1239
Asherson, P., Young, A. H., Eich-Höchli, D., Moran, P., Porsdal, V., & Deberdt, W. (2014). Differential diagnosis, comorbidity, and treatment of attention-deficit/hyperactivity disorder in relation to bipolar disorder or borderline personality disorder in adults. Current medical research and opinion, 30(8), 1657–1672. https://doi.org/10.1185/03007995.2014.915800
Biskin, R. S., & Paris, J. (2012). Diagnosing borderline personality disorder. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 184(16), 1789–1794. https://doi.org/10.1503/cmaj.090618
Bernardi, S., Faraone, S. V., Cortese, S., Kerridge, B. T., Pallanti, S., Wang, S., & Blanco, C. (2012). The lifetime impact of attention deficit hyperactivity disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Psychological medicine, 42(4), 875–887. https://doi.org/10.1017/S003329171100153X
Chen, C. Y., Lin, S. H., Li, P., Huang, W. L., & Lin, Y. H. (2015). The role of the harm avoidance personality in depression and anxiety during the medical internship. Medicine, 94(2), e389. https://doi.org/10.1097/MD.0000000000000389
Cumyn, L., French, L., & Hechtman, L. (2009). Comorbidity in adults with attention-deficit hyperactivity disorder. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 54(10), 673–683. https://doi.org/10.1177/070674370905401004
Distel MA, Carlier A, Middeldorp CM, Derom CA, Lubke GH, Boomsma DI. Borderline personality traits and adult attention-deficit hyperactivity disorder symptoms: a genetic analysis of comorbidity. Am J Med Genet B Neuropsychiatr Genet. 2011;156(7):817–825. doi:10.1002/ajmg.b.31226
Ditrich, I., Philipsen, A. & Matthies, S. Borderline personality disorder (BPD) and attention deficit hyperactivity disorder (ADHD) revisited – a review-update on common grounds and subtle distinctions. bord personal disord emot dysregul 8, 22 (2021). https://doi.org/10.1186/s40479-021-00162-w
Dowson, J. H., McLean, A., Bazanis, E., Toone, B., Young, S., Robbins, T. W., & Sahakian, B. (2004). The specificity of clinical characteristics in adults with attention-deficit/hyperactivity disorder: a comparison with patients with borderline personality disorder. European psychiatry : the journal of the Association of European Psychiatrists, 19(2), 72–78. https://doi.org/10.1016/j.eurpsy.2003.07.010
Ferrer M, Andión Ó, Calvo N, Ramos-Quiroga JA, Prat M, Corrales M, et al. Differences in the association between childhood trauma history and borderline personality disorder or attention deficit/hyperactivity disorder diagnoses in adulthood. Eur Arch Psychiatry Clin Neurosci. 2017;267(6):541–9. https://doi.org/10.1007/s00406-016-0733-2.
Fossati, A., Novella, L., Donati, D., Donini, M., & Maffei, C. (2002). History of childhood attention deficit/hyperactivity disorder symptoms and borderline personality disorder: a controlled study. Comprehensive psychiatry, 43(5), 369–377. https://doi.org/10.1053/comp.2002.34634
Hirsch, O., Chavanon, M., Riechmann, E., & Christiansen, H. (2018). Emotional dysregulation is a primary symptom in adult Attention-Deficit/Hyperactivity Disorder (ADHD). Journal of affective disorders, 232, 41–47. https://doi.org/10.1016/j.jad.2018.02.007
Kuja-Halkola R, Lind Juto K, Skoglund C, Rück C, Mataix-Cols D, Pérez-Vigil A, et al. Do borderline personality disorder and attention-deficit/hyperactivity disorder co-aggregate in families? A population-based study of 2 million swedes. Mol Psychiatry.2021; 26(1):341–9. https://doi.org/10.1038/s41380-018-0248-5.
Lee PH, Feng Y-CA, Smoller JW. Pleiotropy and cross-disorder genetics among psychiatric disorders. Biol Psychiatry. 2021;89(1):20–31. https://doi.org/10.1016/j.biopsych.2020.09.026.
Littman, K. (Feburary, 2021) When Women Battle ADHD and Borderline Personality Disorder. Additude Magazine. Retrieved at: https://www.additudemag.com/adhd-and-bpd-women-borderline-personality-disorder/
Miller CJ, Flory JD, Miller SR, Harty SC, Newcorn JH, Halperin JM. Childhood attention-deficit/hyperactivity disorder and the emergence of personality disorders in adolescence: a prospective follow-up study. J Clin Psychiatry. 2008;69(9):1477–1484
Jacob CP, Romanos J, Dempfle A, et al. Co-morbidity of adult attention-deficit/hyperactivity disorder with focus on personality traits and related disorders in a tertiary referral center. Eur Arch Psychiatry Clin Neurosci. 2007;257(6):309–317. doi:10.1007/s00406-007-0722-6
Matthies S, van Elst LT, Feige B, et al. Severity of childhood attention-deficit hyperactivity disorder–a risk factor for personality disorders in adult life? J Personal Disord. 2011;25(1):101–114. doi:10.1521/pedi.2011.25.1.10
Rüfenacht, E., Euler, S., Prada, P., Nicastro, R., Dieben, K., Hasler, R., Pham, E., Perroud, N., & Weibel, S. (2019). Emotion dysregulation in adults suffering from attention deficit hyperactivity disorder (ADHD), a comparison with borderline personality disorder (BPD). Borderline personality disorder and emotion dysregulation, 6, 11. https://doi.org/10.1186/s40479-019-0108-1
Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry. 2000; 39(11):1424–1431. doi:10.1097/00004583-200011000-00017
Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. J Abnorm Child Psychol. 2012; 40(1):7–20. doi:10.1007/s10802-011-9530-6
van Dijk, F. E., Lappenschaar, M., Kan, C. C., Verkes, R. J., & Buitelaar, J. K. (2012). Symptomatic overlap between attention-deficit/hyperactivity disorder and borderline personality disorder in women: the role of temperament and character traits. Comprehensive psychiatry, 53(1), 39–47. https://doi.org/10.1016/j.comppsych.2011.02.007
Weiner, L., Perroud, N., & Weibel, S. (2019). Attention Deficit Hyperactivity Disorder And Borderline Personality Disorder In Adults: A Review Of Their Links And Risks. Neuropsychiatric disease and treatment, 15, 3115–3129. https://doi.org/10.2147/NDT.S192871